The Painful Or Failing Hip Replacement
The Painful Or Failing Hip Replacement
Hip replacement surgery is generally very successful, with most patients experiencing lasting pain relief and improved mobility. However, some individuals may continue to experience discomfort or stiffness in the months or years following surgery. In other cases, a hip replacement that initially functioned well may begin to loosen, wear, or fail over time.
Not all hip pain after joint replacement indicates failure. In some cases, the pain may be related to soft tissue irritation, referred pain from another part of the body, or changes in joint mechanics. A thorough assessment is essential to determine the cause of your symptoms and whether further treatment is needed.
Dr Darren Paterson provides comprehensive evaluation and management of painful or failing hip replacements, including revision surgery where appropriate.

Common causes of hip pain after replacement
There are many reasons why a hip replacement may become painful, and not all of them involve mechanical failure.
Possible causes include:
- Bursitis or inflammation of the soft tissues around the hip
- Tendon or muscle irritation, especially in the early stages of recovery
- Referred pain from the lower back, pelvis, or sacroiliac joint
- Leg length difference or altered biomechanics after surgery
- Scar tissue or joint stiffness
- Hip instability or clicking sensations
- Implant loosening, wear, or infection
Identifying the source of your discomfort is the first step toward effective treatment. In some cases, simple strategies such as physiotherapy or activity modification may be enough. In others, further investigation and possibly revision surgery may be required.
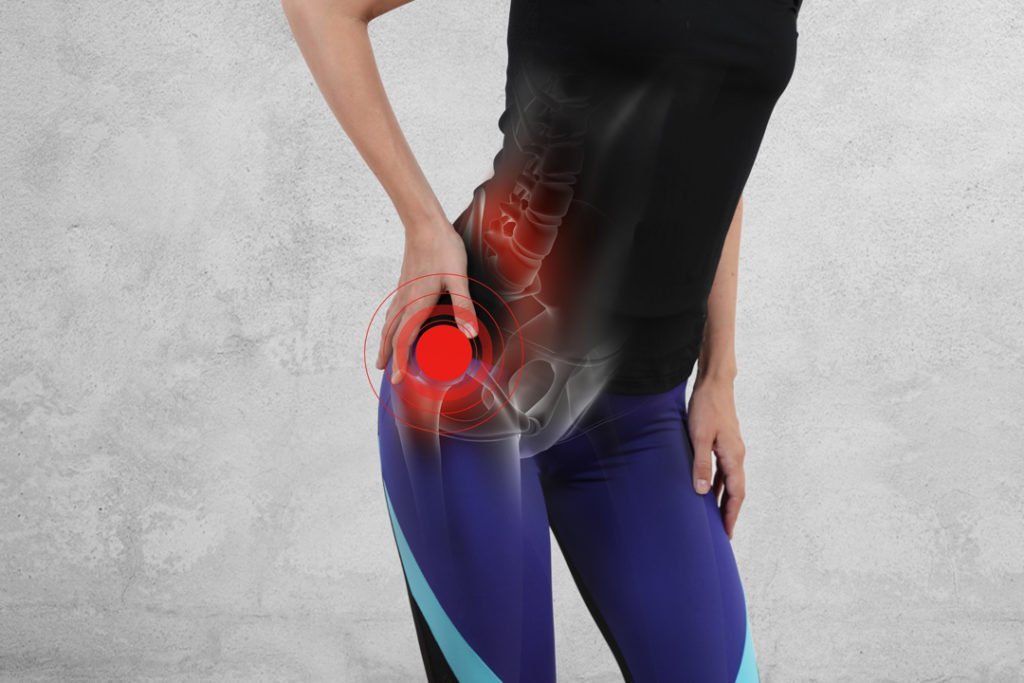
Signs that your hip replacement may be failing
A hip replacement may be considered failing if the prosthetic components are no longer functioning properly or if structural problems are developing within the joint.
Symptoms that may suggest implant failure include:
Ongoing or worsening hip pain, especially during movement
Reduced range of motion or joint stiffness
Swelling, warmth, or redness around the hip
Joint instability, clicking, or episodes of dislocation
Difficulty walking or placing weight on the leg
Changes in leg length or posture
If you are experiencing any of these issues, it is important to arrange a specialist review. Early identification of a failing implant can help prevent further complications and guide appropriate treatment.
What causes a hip replacement to fail?
There are several possible causes of implant-related failure. These include both mechanical issues and biological responses that interfere with the long-term function of the replacement joint.
Common causes include:
- Aseptic loosening: This occurs when the bond between the implant and the surrounding bone weakens over time without infection. It is one of the most common causes of late failure.
- Wear and tear: The artificial joint surfaces may wear down, particularly in younger or highly active patients.
- Joint infection: An infection around the implant (periprosthetic joint infection) can lead to pain, inflammation, and implant loosening.
- Component misalignment or damage: Incorrect positioning or deterioration of the prosthetic parts can affect how the joint functions.
- Periprosthetic fracture: A fracture that occurs near the implant, often after a fall or trauma.
- Dislocation or instability: The ball component may slip out of the socket, especially if the surrounding muscles or ligaments are weak or the implant position has shifted.
How is a painful or failing hip replacement diagnosed?
Dr Paterson will begin by reviewing your medical history, surgical records, and current symptoms. A physical examination will assess your range of motion, joint stability, and areas of tenderness. Imaging and tests will then be used to confirm the cause of the pain.
Investigations may include:
X-rays: To evaluate implant position, bone quality, and signs of loosening
Blood tests: To check for signs of inflammation or infection
Joint aspiration: A small amount of fluid may be drawn from the hip joint to rule out infection
CT or MRI scans: May be used to assess bone integration, surrounding soft tissues, or subtle issues not visible on X-ray
These tests help guide your treatment plan and determine whether revision surgery is necessary.
Treatment options for hip pain following hip replacement
Non-surgical management
- Not every painful hip replacement requires further surgery. In cases where symptoms are mild and the implant is functioning well, non-operative strategies may provide relief.
These may include:
- Physiotherapy to strengthen surrounding muscles and improve joint support
- Anti-inflammatory medications for pain management
- Activity modification to reduce strain on the hip
- Injections to reduce inflammation or treat bursitis
- Use of a walking aid for improved stability and comfort

Revision hip replacement surgery
If the implant is worn, loose, or infected, or if the joint has become unstable or painful despite non-surgical treatment, revision hip replacement surgery may be recommended. Revision surgery involves removing some, or all of the original prosthetic components and replacing them with new implants. This procedure is typically more complex than a first-time hip replacement and requires careful planning and advanced surgical techniques.
Recovery following revision surgery varies depending on the reason for surgery and the complexity of the case. Most patients stay in hospital for a few days and begin physiotherapy soon after. You may require crutches or a walking aid for a period of time, followed by a gradual return to activity.
Dr Paterson performs revision hip replacement using evidence-based surgical techniques and prosthetic systems designed for durability, bone integration, and joint stability.If the implant is loose, worn, infected, or misaligned, revision surgery may be recommended.
Revision knee replacement involves removing the old prosthetic components and replacing them with new implants designed to restore function and address structural problems. This is a more complex procedure than initial knee replacement and requires careful planning. Dr Paterson uses advanced surgical techniques, including patient-specific instrumentation and modern revision systems, to improve accuracy and outcomes.
Recovery after revision surgery may take longer than after a primary knee replacement. Most patients begin physiotherapy shortly after surgery and use crutches or a walker for the first few weeks. Dr Paterson and his team will provide a clear rehabilitation plan and follow-up schedule to support your recovery.
When to seek a review for hip pain after hip replacement
If you have had a hip replacement and are now experiencing ongoing pain, stiffness, or a sense that something is not quite right, it is important to seek a comprehensive assessment. Even if the problem is not implant-related, early diagnosis and treatment can improve your comfort and mobility. Dr Darren Paterson offers detailed evaluation and individualised treatment for patients with painful or failing hip replacements. Whether revision surgery is required or not, the goal is to reduce your discomfort and help you get back to living the life you enjoy.
